Acupuncture and Martial arts in the East and West -
Acupuncture and Martial Arts
- The student chose a teacher, and if he was accepted by the teacher had a very long apprenticeship, to prove (literally through sweat, blood and tears) that he (this was a very male-orientated domain) was worthy to receive instruction.
- This however is not a very useful business model, and is very manpower intensive, inapplicable to a university based system where the priority is to train a lot of people to a safe standard within a certain budget, and:
- As previously described, this can limit the knowledge base to those only personally experienced by the clinician
- In China and East Asia (where the culture of ancestor respect and worship was prevalent) to write down procedures that contradicted those that were written down by their predecessors, bordered on sacrilege, and to openly criticise the written word, frowned upon . However in reality, the teacher / disciple relationship provided a clinical filter, the teacher would often say that 'this technique or point would be "more appropriate" than that point'. In martial arts, this filtering was more blunt - those who applied techniques that were less effective, had a very short lifespan and could not pass them onto the next generation!!!
- Those that wrote the medical texts came from a select group - termed the 'gentlemen physicians'. To be able to write these texts and to support oneself meant you had to come from a certain income stream, and their patients had certain requirements.
- I remember my teacher in China, Professor Wang Ju Yi who was both steeped in Classical Chinese Medicine but was equipped with a very enquiring (one would say 'Western oriented') mindset and who was willing to question (in a very respectful way) the classics discussed the history of channel palpation. In his opinion the physical palpation of the channels was commonplace in the time when the original classics were written. Although the classics were written between 1,500 to 2,500 years ago, no extant copies remain - the physical copies that are available today are usually Song or Qing dynasty copies and commentaries, which date from only about 1,000 years ago. However during the feudal period, the physical touching of patients (especially those from a higher social class) was frowned upon and emphasis placed on symptom taking, together with pulse and tongue diagnosis. He was of no doubt that the palpation was carried on by the lower class doctors who treated the general population - however they rarely wrote the books!!! On the plus side, the specialisations of pulse, tongue and symptom taking was raised to an entirely new dimension.
- For further insights into Channel Palpation click onto short 20 minute video below. Alternatively please go to the Applied Channel Theory website, by clicking here, where you will find numerous articles, podcasts and further resources.
I believe that there is already much crossover between Traditional East Asian Medicine (TEAM) and the West:
- Dry needling (also known as Intra Muscular Stimulation IMS) is where a thin, solid filiform needle is inserted into the body to treat dysfunction of skeletal muscle and connective tissue, to improve pain control and reduce muscle tension. The term Dry Needling was originally attributed to Dr Janet Travell MD (who was physician to the Whitehouse and to 2 presidents - Kennedy and Linden-Johnson) who dedicated her life developing the theory of, and practice of, myofascial Trigger Points to treat pain. People often state it is different to acupuncture since it is scientifically based and does not rely on energy meridians. However, again context is everything. There are many types of channels in Chinese Medicine, which include the Jing Luo (which are the meridian lines you often see on acupuncture charts and models) but also the Jing Jin (or channel sinew meridians) which are more akin to the myofasical planes seen, for example, in the Anatomy Trains book by Tom Myers. Treatment here often involves treating the local painful points (called Ah Shi or 'Oh Yes").
- Fascial tools, e.g. Graston technique (often used by Chiropractors) and IASTM (Instrument Assisted Soft Tissue Mobilization, often used by Physiotherapists) are methods of instrument assisted mobilization to help reduced pain, identify restricted areas, break down scar tissue, improve local circulation and promote healing - which is basically a modern version of Gua Sha. For more information by a specialist in this field, Dr Arya Nielsen PhD, - click here
- Myofascial Decompression (MFD) Techniques where negative pressure is instigate by applying suction sups to an area of the body, thereby drawing skin and fascia away from the midline thereby altering blood flow and metabolic exchanges, drawing out toxins and reducing pain by endorphin release. This is basically Ba Guan, or cupping.
As has been eluded to, there is much similarity in the training, philosophy and discipline required between traditional martial arts and traditional Chinese medicine.
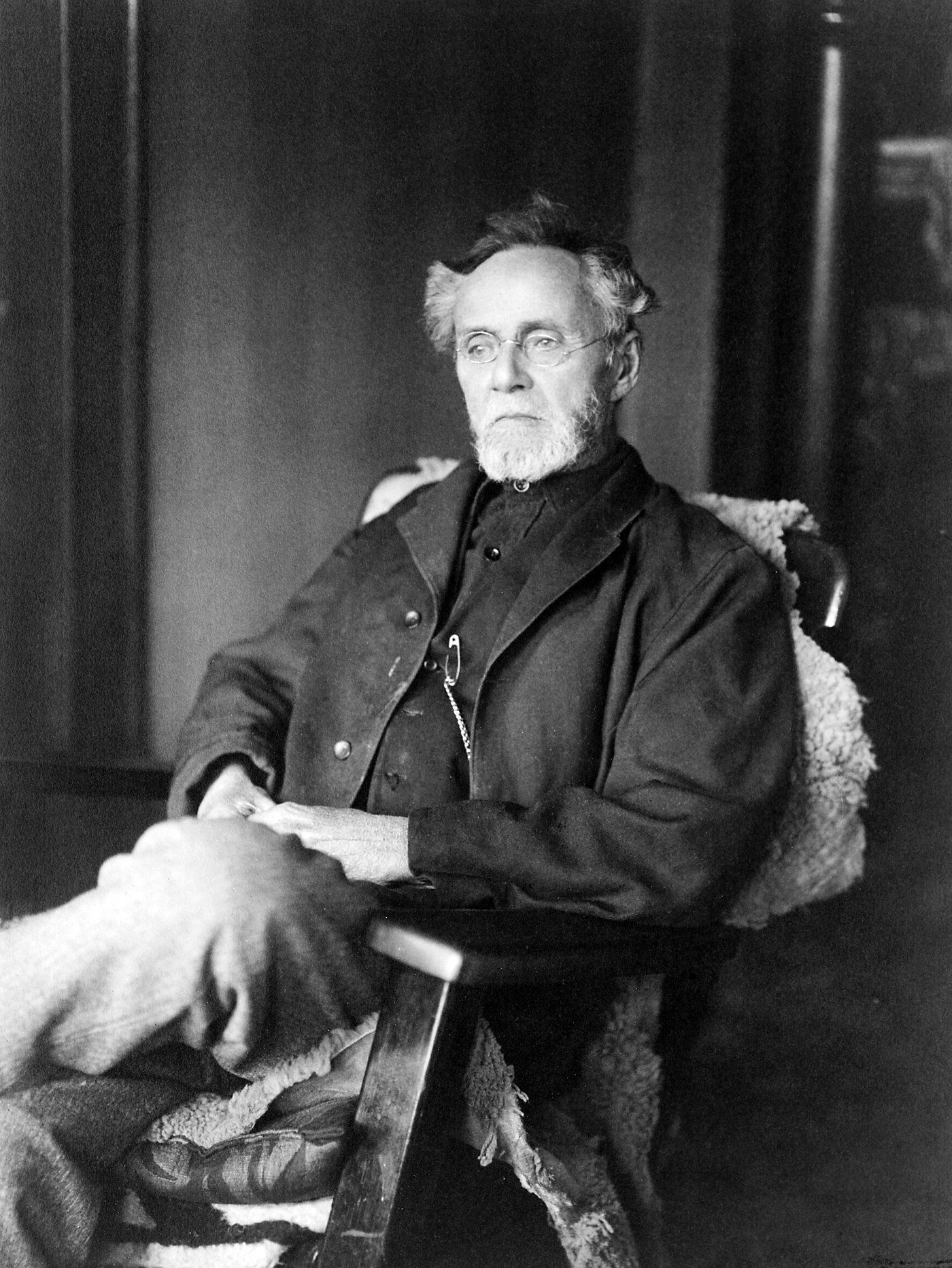
You may recognise a much younger me training with my teacher, Mike Finn Sensei, in empty hand techniques
References
Greenhalgh T (2014) How to Read a paper, the basics of Evidence Based Medicine, 5th Ed, BMJ Books, Chichester, West Sussex (hard copy and Kindle eBook)
Hruby, J and Hoffman, K (2007), Avian influenza, an osteopathic component to treatment, Osteopathic Medicine in Primary Care, 2007; 1 : 10, Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1939852/
Markel H et al (2007) Nonpharmaceutical Interventions Implemented by US Cities during the 1918-1919 Influenza Pandemic, JAMA, Vol 298 (19), Available at https://jamanetwork.com/journals/jama/fullarticle/208354
Miller D (2016) Introduction to Traditional Chinese Medicine, Integrative Health Network, Available at: https://www.youtube.com/watch?v=WKpKEYo3me0
Nielsen, A (2012), Gua Sha: a traditional technique for modern practice, 2nd Ed, Churchill Livingstone, Edinburgh (Available as a hardback and eBook)
Root Bernstein, R and M (1998) Honey, Mud, Maggots and other medical marvels: the science behind folk remedies and old wives' tales, Houghton Mifflin Company, Boston (available as a book and on audible)